About Me
ডাঃ মাসুদ হোসেন
আসসালামুয়ালাইকুম, আমি ডাঃ মাসুদ হোসেন। আমি গভমেন্ট রেজিস্ট্রার প্রাপ্ত হোমিওপ্যাথিক ডাক্তার। আমার চেম্বার চট্টগ্রাম আগ্ৰাবাদ। আমি ক্লাসিক্যাল হোমিওপ্যাথি চিকিৎসা পদ্বিতিতে চিকিৎসা দিয়ে থাকি।
আমার লক্ষ্য হলো হোমিওপ্যাথিকে আধুনিকতার ছোঁয়া ও নতুনত্বের ছোঁয়া দেয়া। হোমিওপ্যাথি নিয়ে আমার চিন্তা ধারা সূদর প্রসারিত। হোমিওপ্যাথি হলো প্রাকৃতিক নিরাময় ব্যবস্থা।যা বহু শতাব্দী ধরে চলে আসছে। কোনো পদার্থ সুস্থ ব্যক্তির দেহে রোগের যে উপসর্গের সৃষ্টি করতে পারে তেমনি একই উপসর্গে আক্রান্ত কোনো ব্যক্তিকে সুস্থ করে তোলে। হোমিওপ্যাথি বাহিরে ও ভিতরে উভয়ই ক্ষেত্রে চমৎকার কাজ করে।
অর্থাৎ রোগকে সমূলে নির্মূল করে। পেঁয়াজ এর কথা কল্পনা করা যাক -নাক ও চোখ দিয়ে পানি পড়া। এখন ইতিমধ্যেই অ্যালার্জি ও সর্দি থেকে এ ধরনের লক্ষন পেয়েছেন তাহলে পেঁয়াজের(এলিয়াম সেপা) ছোট একটি ডোজ আপনার লক্ষন গুলো হ্রাস করে সুস্থ করে তুলতে পারে। হোমিওপ্যাথি শুধু ব্যক্তির লক্ষন হ্রাস করে না বরং ব্যক্তির সামগ্ৰিক স্বাস্থ্যর উন্নতি সাধন করে। হোমিওপ্যাথির আরো অনেক সুবিধা রয়েছে তার মধ্যে অন্যতম হলো :
- পার্শ্ব প্রতিক্রিয়া মুক্ত।
- নির্দিষ্ট রোগ নিরাময়ের সাথে সাথে সামগ্ৰিক স্বাস্থ্যর উন্নতি সাধন করে।
- দীর্ঘস্থায়ী রোগের জন্য কার্যকরী।
- সকল বয়সী মানুষের জন্য নিরাপদ।
- কম ব্যয়বহুল।
হোমিওপ্যাথি মানুষের প্রাকৃতিক নিরাময় ক্ষমতাকে উদ্দীপিত করে স্থায়ীভাবে সুস্থ করে তুলতে সাহায্য করে।
আসলেই হোমিওপ্যাথি হলিস্টিক মেডিসিন। সুস্থ থাকতে আমাদের সকলের উচিত হোমিওপ্যাথি চিকিৎসা গ্ৰহন করা। হোমিওপ্যাথি নিয়ে মন্তব্য না করে আসুন আমরা হোমিওপ্যাথি চিকিৎসা পদ্ধতি সম্পর্কে জানতে চেষ্টা করি।
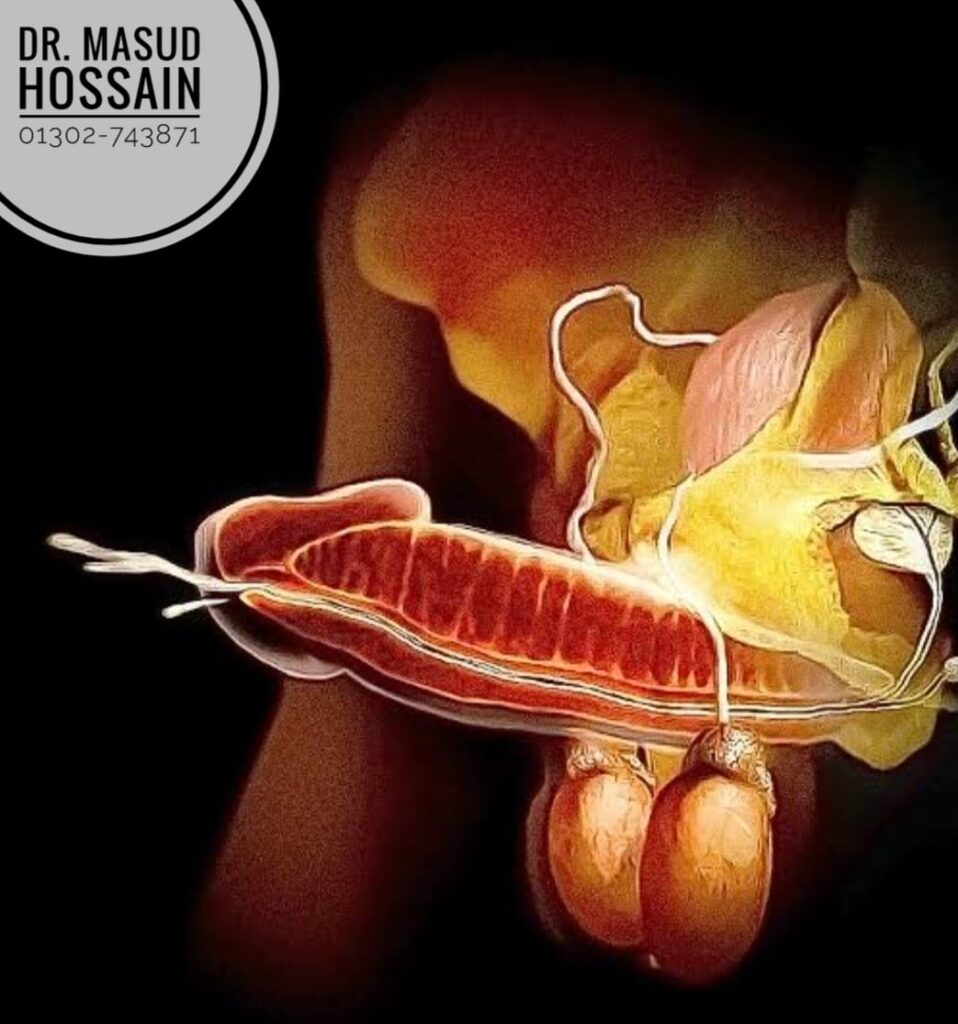
আমি যৌন রোগ বিশেষজ্ঞ, জার্মানির ক্লাসিক্যাল হোমিও চিকিৎসা পদ্ধতিতে চিকিৎসা দেই এবং অরিজিনাল জার্মানির ঔষধ দিয়ে কম্বিনেশন করে ডোজ দেই তাই আমি চট্টগ্রামের সেরা হোমিও ডাক্তার। আমি সর্বনিম্ন দুই /আড়াই মাসের ঔষধের ডোজ দেই। আমার ডোজগুলো সাধারণত পুরুষের টেস্টোস্টেরন হরমোন কমে গেলে, পুরুষের অন্ডকোষ ঝুলে গেলে,লিঙ্গ ছোট ও চিকন হয়ে গেলে, সহবাসের সময় লিঙ্গ শক্ত না হলে, সহবাস করার সাথে সাথে বীর্য আউট হয়ে গেলে এবং পুরুষাঙ্গ মোটা তাজা করার জন্য স্থায়ীভাবে কার্যকরী হয় আমি অভিজ্ঞ হোমিও ডাক্তার চট্টগ্রাম।
তাছাড়া পুরুষের অন্ডকোষের ভেরিকোসিল,এপিডিডাইমেল সিস্ট,অন্ডকোষের টিউমার, প্রস্রাবের আগে পরে ধাতু ক্ষয় , অতিরিক্ত হস্তমৈথুনের কারণে পুরুষত্ব নষ্ট হয়ে গেলে, লিঙ্গের স্বাস্থ্য বৃদ্ধি করতে, সিফিলিস ও গনোরিয়া ভালো করতে হাই পটেন্সি ঔষধ ব্যবহার করে থাকি চর্ম ও যৌন রোগ বিশেষজ্ঞ । আপনি চাইলে আমার চেম্বারে আসতে পারেন অথবা চাইলে কুরিয়ার সার্ভিসের মাধ্যমে হাতে হাতে পৌঁছে দিবো ইনশাল্লাহ।
কুরিয়ার সার্ভিসের মাধ্যমে প্রবাসী বাংলাদেশীদের কাছে আমি প্রচুর ঔষধ পাঠাই। হোমিও ঔষধ প্রোপারলী প্রয়োগ যৌন স্থায়ীভাবে ভালো হয়ে যায় কিন্তু কোন সাইড এফেক্ট হয় না। আমার একটি ইউটিউব চ্যানেল আছে এবং ফেসবুক গ্ৰুপ আছে । বিভিন্ন প্রকার জটিল ও কঠিন রোগ নিয়ে আলোচনা করি। আপনি জয়েন্ট করলে রোগ সম্পর্কে অনেক কিছু জানতে পারবেন।
যৌন সমস্যা, চর্মরোগ, এলার্জি, একজিমা,অ্যাজমা,সোরোসিস, টিউমার, আইবিএস,গ্যাসট্রাইটিস,পিত্ত পাথর,কিডনি পাথর, লিভারের সমস্যা,এপিডিডাইমাল সিস্ট,ভেরিকোসিল, ওভারিয়ান সিস্ট,ফাইব্রোয়েড,ন্যাজাল পলিপস,পাইলস, ফিস্টুলা,এনাল ফিসার,লাইপোমা,জন্ডিস, সাইনোসাইটিস, আলসার, নারী ও পুরুষের বন্ধ্যাত্ব,ব্রন,ক্যান্সার সহ ক্রনিক রোগের অরিজিনাল জার্মানির হোমিও ঔষধ দ্বারা চিকিৎসা করে থাকি।












Imo & Whatsapp
+8801302-743871 +880190-7583252
ঠিকানা
আগ্রাবাদ, এক্সেস্ রোড়, বেপারী পাড়া, চট্রগ্রাম